Feeling nervous before your first session is completely normal, and you’re not alone in this experience. Many people have concerns about sharing personal information, and it can be daunting to step into a new environment. But the good news is that this type of therapy can be incredibly supportive, even if you’re feeling unsure at first.
In this post, we’ll guide you through how this therapy can help you manage stress from work or family life in Burleson, explain what types of therapy groups are available at Mind Above Matter, and provide some helpful tips to prepare for your first session.
Work and family stress can have a significant impact on your mental health. Balancing deadlines, responsibilities, and relationships can be overwhelming. If this stress isn’t managed, it can lead to burnout, anxiety, or even depression. That’s where outpatient therapy comes in.
In Burleson Outpatient Group Therapy, you’ll have the opportunity to talk about the daily stressors you face and gain support from others who may be going through similar struggles. You’ll learn effective coping strategies, such as mindfulness, setting boundaries, and improving time management, all of which can help you reduce stress and maintain a healthy balance in your life.
One of the biggest benefits of group therapy is the sense of community it provides. You’ll connect with others in Burleson who understand what you're going through, which can help alleviate feelings of isolation. Moreover, as you share your challenges and successes, the group can help hold you accountable for implementing stress-reducing strategies. Support from others can motivate you to make positive changes in your everyday life.
.png)
At mental health services Burleson TX groups are tailored to address a variety of needs. Whether you’re dealing with grief, trauma, anxiety, or general life challenges, there’s a group for you.
Some groups are focused on specific issues, such as grief, trauma, or anxiety. These specialized groups provide targeted support, enabling participants to connect with others facing similar challenges. If you’ve experienced a loss, are navigating the aftermath of trauma, or are managing anxiety, a specialized group can offer the focused attention you need.
If you choose a specialized group, you’ll find that the members share similar experiences, making it easier to connect and feel understood. For example, in a grief group, you can openly discuss the unique challenges of losing a loved one with others who are also grieving. This shared understanding can be comforting and help accelerate the healing process.
For those unsure where to start or managing multiple concerns, a general therapy group may be the right fit. These groups address a broad range of life challenges, from relationship difficulties to work stress, and offer support to anyone seeking to improve their mental well-being. General groups can provide a sense of community while allowing you to explore different aspects of your mental health clinic Burleson TX
It’s natural to feel nervous about attending your first group therapy session. The idea of opening up in front of strangers can be intimidating, but remember that everyone in the group is there to support one another, and no one will judge you. Here’s how you can prepare:
The first thing to keep in mind is that it’s okay to be nervous. Most people feel the same way before their first session, and that nervousness is a sign that you’re taking a step toward healing. Outpatient Group Therapy Burleson is designed to be a safe and supportive space, so take comfort in knowing that you’re not alone.
Before your first session, take a moment to reflect on why you’re seeking therapy. What are your goals? What do you hope to achieve from the experience? If it helps, write down any thoughts, feelings, or concerns you’d like to share. Journaling can be a great way to get your emotions out and begin processing them before the session starts.
Your first session will likely start with introductions and a brief overview of group rules. You’ll be guided by a trained therapist who will set the tone and ensure that everyone feels comfortable. Don’t worry about sharing immediately; most groups allow you to ease into the process. You can take your time and participate when you’re ready.
If you’re feeling anxious, try arriving a little early to get settled. Taking deep breaths or using a grounding technique can help calm your nerves. It’s also helpful to remind yourself that you don’t have to share anything you’re not ready to. Group therapy is about your pace participate as much or as little as you need.
Starting Mind Above Matter can be a little intimidating, but it’s also an opportunity for growth, healing, and connection. Whether you’re managing stress from work or family life, addressing specific issues like grief or trauma, or simply looking for support, group therapy can be a powerful tool in your mental health journey.
If you’re nervous about attending your first session, remember that it’s completely normal to feel that way. With time, you’ll likely find that the group becomes a supportive environment where you can share, listen, and grow.
In Burleson, group therapy is a valuable resource for managing stress, navigating grief, and addressing personal challenges.
Ready to take the first step in your recovery? Contact us today to learn more about our outpatient therapy sessions and how they can help you manage stress, work through grief, or address other challenges you may be facing.
If you’re struggling with addiction and considering therapy, you may be wondering: “Will it work if I’m not comfortable sharing my personal experiences with others?” It’s a common concern, but the short answer is yes, it can still be beneficial even if you’re not ready to share right away.
This type of therapy can play a vital role in your recovery, providing a sense of community, support, and accountability. In this post, we’ll explore how it works, how it can help you, and how to decide if it’s the right fit for you, particularly for those in Burleson, TX.
Outpatient Group Therapy Burleson TX is a treatment option where individuals recovering from addiction attend therapy sessions in a group setting, while living at home and maintaining their daily routine. This approach offers flexibility and can be a less intensive alternative to inpatient programs.
In group therapy, a licensed therapist facilitates discussions, helping participants learn coping strategies, share experiences, and support one another. While sharing is encouraged, it’s never required. Group members are there to offer support, listen, and learn from each other, creating a safe space for everyone.
If you’re not comfortable sharing your personal story in a group setting, that’s completely okay. In fact, it’s common for people to feel hesitant to open up, especially in the early stages of recovery. The good news is that group therapy can still be incredibly valuable, even if you’re not ready to share everything.
The key to group mental health clinic Burleson is creating a supportive environment where participants listen without judgment. While sharing your personal experiences is encouraged, it’s always voluntary. If you prefer to listen and learn from others before speaking up, that’s perfectly fine. Your participation in the group is valuable, whether you’re speaking or just listening.
Many people find that as they attend more sessions, they become more comfortable with the group. Trust is built gradually, and you may find that, over time, you feel more open to sharing. The goal is not to pressure you, but to allow you to heal at your own pace.
In group therapy, you don’t have to be the one doing all the talking. Some people contribute by offering support and encouragement to others. Others may prefer to observe and reflect on what they’re hearing. Both roles are important in fostering a healthy group dynamic, and no one is forced to share personal details if they’re not ready.

Outpatient group therapy offers several benefits that can enhance your recovery journey, especially if you’ve been struggling with substance abuse or addiction in Burleson, TX.
Addiction can often make people feel isolated, as though no one understands their struggles. In group therapy, you’ll meet others who are going through similar experiences. This shared understanding can help you feel less alone and more connected to others. You’ll find that the support of others in the group can make a huge difference in your healing process.
Take Sarah from Burleson, for example. She had been struggling with alcohol addiction for several years and was hesitant to seek help because she felt isolated in her struggles. When she joined a local outpatient group therapy program, she initially found it difficult to open up. Over time, as she listened to others and heard their personal stories, Sarah became more comfortable and began sharing her own journey. The support she received from others in the group not only helped her stay accountable but also made her feel understood and empowered. Today, she’s continuing her recovery with the support of her community.
One of the key advantages of group therapy is the accountability it fosters. By participating in group discussions and setting goals with others, you’ll feel motivated to stick to your recovery plan. The group setting encourages progress and encourages everyone to stay on track.
The Outpatient Group Therapy Burleson, you’ll have the opportunity to learn valuable coping strategies and tools for handling triggers, cravings, and emotional challenges. These skills are shared through group discussions and activities led by a trained therapist. You’ll also benefit from hearing about others' experiences and learning what has worked for them in their own recovery.
While the group provides peer support, the therapist is there to guide and offer professional advice. The therapist can help you work through personal challenges, provide tailored coping strategies, and navigate the complexities of recovery. Having professional guidance in a group setting can be incredibly helpful in strengthening your recovery plan.
Outpatient group therapy can be a fantastic option for many people, but it’s important to understand whether it’s the best fit for your unique situation.
If you’re struggling with mild to moderate addiction or substance abuse, outpatient group therapy could be an excellent fit. It offers a balance of structure and flexibility, ideal if you have other responsibilities, such as work or family commitments, to manage. Outpatient therapy also works well for people who are transitioning from inpatient treatment and want ongoing support.
However, if you’re dealing with severe addiction or have experienced multiple treatment failures in the past, outpatient therapy might not be enough on its own. In such cases, you may need a more intensive treatment program, such as inpatient rehab or a detox facility. A professional evaluation can help determine if a higher level of care is necessary.
The best way to determine if mental health services Burleson TX is right for you is to consult with a therapist or treatment center. They can assess your current struggles, history with addiction, and overall mental health to recommend the most appropriate course of treatment. In Burleson, TX, local resources can help guide you through this decision. You can contact trusted outpatient therapy providers in Burleson for a personalized consultation.
Mind Above Matter can be a powerful tool in your recovery journey, especially if you're struggling with addiction or substance abuse in Burleson, TX. Even if you’re not comfortable sharing personal experiences right away, the supportive environment and peer connections will help you feel less isolated and more motivated. Whether you’re just starting your recovery or need ongoing support, group therapy can offer the tools, accountability, and sense of community you need to succeed.
If you're unsure whether outpatient group therapy is the right choice for you, consider reaching out for a consultation with a local professional who can help you make the best decision for your recovery.
Participating in a group setting can be a powerful tool for personal growth, helping individuals improve communication skills and overcome feelings of isolation. Whether you're struggling with social anxiety or loneliness, or just want to connect more effectively with others, this collaborative environment offers a unique opportunity to work through challenges in a supportive way. In this post, we’ll explore how these sessions work, how to track your progress, and how they can help you build stronger connections with those around you.
In a group setting, the Burleson Outpatient Group Therapy plays a crucial role in creating a space where every participant feels heard and supported. Here’s how they do it:
Therapists begin by establishing ground rules that promote openness, respect, and confidentiality. This creates an environment where everyone feels comfortable sharing their thoughts and emotions. When people feel safe and supported, they are more likely to open up and engage in discussions.
One of the mental health clinic Burleson TX main goals is to ensure everyone has a chance to speak. They gently encourage quieter members to share their experiences and ensure that no one dominates the conversation. This balance helps everyone feel included, valued, and part of the group.
Group therapy involves a mix of personalities, and therapists are skilled at managing these dynamics. If any tension or conflict arises, the therapist will step in to guide the conversation, keeping it respectful and productive. This helps ensure that everyone’s voice is respected and the focus remains on personal growth.
.png)
It can sometimes be hard to tell if group therapy is making a difference, but several signs show it’s working:
One of the first changes you'll notice is an improvement in how you communicate. Group therapy encourages you to express your thoughts, feelings, and needs more clearly. Over time, you may find that you’re able to communicate more effectively not only in group settings but also in your day-to-day interactions with others. For example, if you're in Burleson and you’ve struggled with making small talk at work, group therapy can help you become more comfortable in conversations, giving you the confidence to speak up when needed.
Another key indicator is how you feel emotionally. Outpatient Group Therapy Burleson can help reduce anxiety, stress, and loneliness. As you build connections with others, you may notice a sense of relief from feelings of isolation. For instance, a client in Burleson reported feeling significantly less isolated after attending group therapy, as they realized they weren’t alone in their struggles.
Feedback is a great way to gauge your progress. Therapists will often provide feedback on your growth, pointing out areas where you've made strides. Group members may also offer insights or support, which can help you see how much you've improved.
Group therapy doesn’t just help with internal growth; it’s also a great way to improve your ability to connect with others. Here’s how it can help:
If social anxiety or fear of judgment has held you back, group therapy can be incredibly helpful. By regularly practicing communication in a supportive setting, you'll build confidence in your social interactions. For example, one participant in our Burleson group sessions shared that they had never felt confident speaking in front of others. However, after attending several sessions, they not only felt more at ease in mental health services Burleson TX but also gained the courage to speak up at work meetings.
Group therapy is a great space to learn and refine communication skills. Therapists teach participants how to listen actively, express themselves assertively, and handle difficult conversations with ease. These strategies will help you connect more effectively with others, whether you’re negotiating with a colleague in Burleson or having a tough conversation with a friend.
One of the most powerful aspects of Mind Above Matter is realizing that you're not alone in your struggles. When you hear others share similar experiences, it can reduce feelings of loneliness and help you feel understood. For instance, a participant from Burleson mentioned that after hearing others talk about their challenges with social anxiety, they felt a deep sense of connection and support. This realization helped them open up and engage more fully in the group.
Participating in a supportive group setting offers an incredible opportunity to enhance communication skills, gain emotional support, and reduce isolation. Providing a safe, structured environment for individuals to share and learn fosters personal growth and stronger connections with others. Whether you’re in Burleson or any other community, this collaborative approach can be a powerful tool to improve how you connect with the world around you.
If you’re ready to start your journey and see how group therapy can benefit you, reach out to a professional therapist today. You’ll be surprised at how much you can learn about yourself and others in a group setting, and how it can enhance your ability to communicate and connect.
Deciding between group sessions and individual counseling can feel overwhelming, but it doesn't have to be. Both options offer unique benefits, and the right choice depends on your personal needs, preferences, and goals. Whether you’ve already tried individual counseling or are just starting your mental health journey, it’s important to understand how each option works and what might be most helpful for you. In this post, we’ll answer some of the most common questions to help you make an informed decision.
Outpatient Group Therapy Burleson TX is a treatment method where several people come together to work on their mental health with the guidance of a trained therapist. It typically involves 6-12 participants, and the sessions address issues such as anxiety, depression, addiction, and relationship difficulties. Group therapy offers a unique opportunity to connect with others, share experiences, and receive feedback in a supportive, structured environment.
A licensed therapist or group facilitator leads the sessions. They ensure the group stays on track, provide professional guidance, and create a safe space for participants to share and learn. The therapist helps guide discussions, mediate group dynamics, and offer insights that encourage personal growth for everyone involved.
Most outpatient group sessions include around 6 to 12 participants. Group size can vary depending on the center and the group's specific focus. Smaller groups often allow for more personalized attention, while larger groups offer a wider variety of perspectives and experiences. Either way, group sessions are designed to foster a sense of community and belonging, regardless of group size.
The size of the group can influence your experience. Smaller groups tend to allow for more one-on-one time with the therapist and deeper personal connections between members. Larger groups can offer a broader range of experiences and insights, which can be just as helpful for seeing things from different angles. It ultimately depends on your preference and what you feel will work best for your progress.
If individual counseling hasn’t worked for you in the past, participating in a group session might offer something different. It’s possible that, in individual counseling, you didn’t feel connected or supported enough by your counselor, or that you struggled with a lack of social interaction. Group sessions give you the opportunity to learn from others and receive feedback in real-time, which can make a big difference in your progress.
For many people who have struggled with individual therapy, group therapy provides a renewed sense of hope. One of the greatest benefits is the social support and shared experiences that can help you feel less isolated. By listening to others and sharing your own story, you can gain new insights and learn from different coping strategies. Additionally, the Outpatient Group Therapy Burleson offers a safe place to practice social skills, improve communication, and build confidence in your relationships with others.
.png)
Choosing a group session starts with self-reflection. Think about how comfortable you are with sharing personal experiences in a group setting. If you’re someone who enjoys hearing from others and feels energized by group interactions, you may thrive in this environment. However, if you prefer more in-depth, private conversations with a counselor, individual counseling might feel like a better fit.
It's also important to think about your specific goals. If you're looking for emotional support and the opportunity to learn from others, participating in a group session may be ideal. On the other hand, if you're dealing with complex personal issues or prefer a more tailored, one-on-one approach, individual counseling might be the better route.
Individual counseling focuses solely on your personal experiences and goals. You have one-on-one time with a therapist, which allows for more in-depth exploration of your issues. This option is great if you need a more personalized approach and want to work through specific challenges in detail. Mental health clinic Burleson, however, offers a chance to interact with others who may be going through similar struggles. You get to hear from multiple people, gaining different perspectives and learning from their experiences. It also helps to build social support and offers the opportunity to practice social skills in a safe space.
If group and individual therapy aren't quite what you're looking for, there are other options available. For example, couples or family therapy might be beneficial if you're struggling with relationship dynamics. Online therapy is another option that offers more flexibility if in-person group or individual therapy doesn't work with your schedule.
Consider the case of Emily, who had been attending individual therapy for several months but felt like she wasn’t making much progress. She struggled with social anxiety, and while talking to her therapist was helpful, she still felt isolated and alone in her experiences. Emily decided to give group therapy a try, and it made all the difference. Hearing from others who shared similar challenges and getting feedback from her group members gave her new strategies to manage her anxiety. She found comfort in knowing she wasn’t the only one facing these struggles, and it gave her the motivation to continue working on her mental health.
Mind Above Matter group of therapy and individual counseling ultimately come down to your personal preferences and goals. Group therapy can be a powerful tool for those who need social support, community, and diverse perspectives. It’s also a great option if you’ve tried individual therapy without seeing the results you hoped for. However, individual counseling remains a great choice for those who prefer one-on-one time with mental health services Burleson TX to explore personal issues in depth.
If you're still unsure about which path is right for you, consider speaking with a local therapist in Burleson, TX, who can help guide you through the decision-making process. No matter which option you choose, taking the first step toward seeking help is always a positive move.
Ready to explore your therapy options? Reach out to a local therapist today to discuss whether group therapy or individual counseling would be the best fit for your needs!
The holiday season and mental health challenges often go hand-in-hand. This time of year is consistently painted as a period of uninterrupted joy and peace. However, for a significant number of individuals, this expectation creates immense pressure, marking a peak in holiday stress and mental health struggles, anxiety, and even depressive symptoms. The gap between the idyllic scenes we see in media and the reality of navigating complex family dynamics, financial pressures, and overwhelming scheduling conflicts can be profound. At Mind Above Matter (MAM), we want to validate that it’s completely normal to feel overwhelmed. You are not alone in this feeling.
This guide will explore the primary factors that contribute to holiday mental health strain, recognizing that the challenge isn't the festive season itself, but the increased emotional and logistical load it places on our already busy lives. We will discuss why managing expectations and setting compassionate boundaries are necessary components of self-care required to keep you "Closer to Whole" through the end of the year and beyond.
Understanding the sources of stress is the first step toward managing them. The intense, compounded nature of holiday demands typically falls into three main areas that tax both your mind and your resources.
The most immediate and pervasive source of stress is often financial pressure. There is a deep-seated cultural expectation to purchase extravagant gifts, host large, elaborate meals, and fund expensive travel. This consumer-driven pressure can lead to significant anxiety, debt, and subsequent feelings of shame or failure.
Additionally, the logistical strain of managing multiple schedules, coordinating travel across states or cities, and preparing homes for guests disrupts the consistent routines that are vital for maintaining mental stability, especially for those managing existing mood disorders or anxiety.
The holidays frequently involve interacting with challenging or estranged family members, resurrecting old family conflicts, or navigating new losses. For those who are grieving, lonely, or managing chronic conditions, the forced cheer and intense focus on "family" can unintentionally amplify existing feelings of isolation or sadness. This emotional burden is exhausting, demanding energy that is better spent on personal wellness and healing. It is crucial to remember that you do not owe anyone a performance of happiness.
The holidays are inherently disruptive to the physical routines that form the foundational pillars of mental health: getting adequate sleep, eating regular, nutritious meals, and maintaining exercise habits. Late-night parties, travel across different time zones, and the abundance of rich foods destabilize the body’s chemistry and circadian rhythm. This physical disruption is a major pillar of stress, leading directly to:
Successful mental health management—for every age group, from the adolescents in our iMatter school programs to our geriatric clients—relies heavily on consistency. This includes getting adequate sleep, eating regular, nutritious meals, and maintaining exercise habits. The holiday season is inherently disruptive to these foundational pillars. Late-night parties, travel across different time zones, and the abundance of rich foods can destabilize the body’s chemistry and circadian rhythm, leading to:
In the rush to accommodate the needs and expectations of others, personal self-care often drops off the schedule entirely. Therapy appointments are postponed, quiet time for meditation is skipped, and, critically, medication might be taken irregularly due to travel or scheduling changes. This erosion of protective habits leaves individuals highly vulnerable to anxiety, burnout, and relapse. We must reframe self-care during the holidays not as a luxury or a reward, but as the essential fuel required to get through the extra demands of the season.
One of the most effective holiday mental health tips we can offer is learning to set and enforce compassionate boundaries. This is about self-preservation, not rejection.
Boundary setting is the most powerful tool for mitigating stress. This process begins by identifying your "non-negotiables"—the few elements of your routine that must be protected, regardless of external pressure.
Your Non-Negotiable Checklist:
It is perfectly acceptable to decline an invitation that will overtax your energy reserves. Furthermore, the Gentle Exit strategy—allowing yourself to leave a gathering early when your battery is low, without feeling obligated to give a detailed explanation—is a vital skill for maintaining emotional equilibrium during crowded or chaotic events. A simple, polite "I can only stay for an hour, but I wanted to make sure I saw you" communicates your boundary clearly before the event starts.
Much of the holiday stress and mental health strain stems from the pursuit of a perfect, idealized holiday—the spotless house, the perfect gifts, the flawless family interaction. This unattainable, movie-ready goal inevitably sets us up for disappointment and feelings of inadequacy. Instead, focus on shifting the goalpost from perfection (the appearance of success) to meaningful connection (the depth of presence). Lowering standards for décor, cooking, or gift-giving frees up immense mental energy for genuine engagement with the people you care about.
If existing family traditions are historically sources of pain or stress, empower yourself to introduce one new, small, low-stress tradition. This could be a ritual that focuses purely on comfort or joy. Examples include:
This takes back agency and creates a welcome buffer against the weight of old, stressful expectations. The goal is to design a holiday experience that fits your current life and mental health needs, not the one dictated by external pressure or past memories.
The holiday season is temporary. While navigating this period requires intention, preparation, and self-compassion, remember that you are capable of managing these challenges by prioritizing your mental health. Small, consistent acts of self-care—from maintaining sleep to setting a necessary boundary—are powerful defenses against burnout. Be gentle with yourself throughout the entire month of December, and remember these mental health holidays tips.
If the stress, anxiety, or depressive symptoms feel too heavy to manage alone, please know that comprehensive, structured care is here in the DFW area. At Mind Above Matter, we understand the unique pressures of this season. Our evidence-based programs, including our Partial Hospitalization Program (PHP) and Intensive Outpatient Program (IOP), are designed to provide the clinical structure and support needed for immediate stabilization, healing, and sustained recovery.
Do not let holiday stress derail your stability.
If you or a loved one needs professional assessment or support to maintain your mental health during the holidays, please reach out for a confidential consultation. Mind Above Matter is here to help you find your path forward.
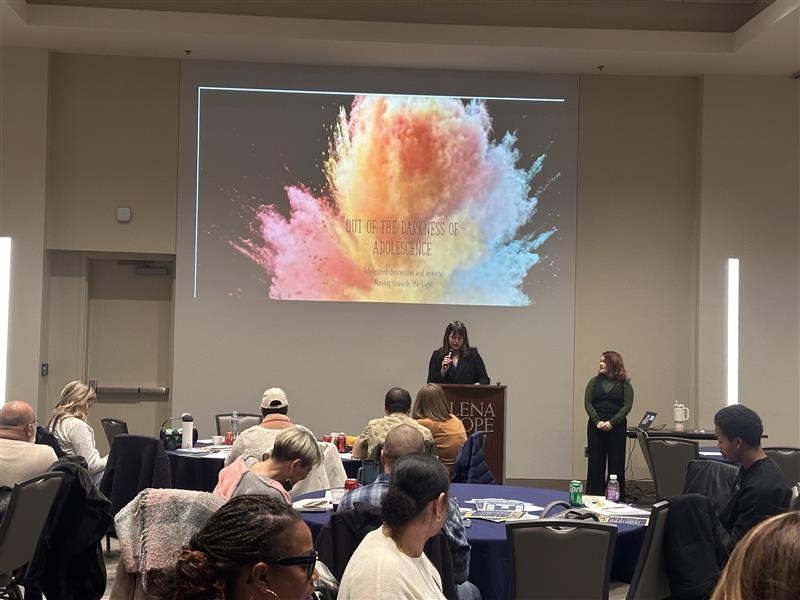
Fort Worth, TX – February 21, 2025 – The highly anticipated 3rd Annual Resiliency & Recovery Conference of Fort Worth, a cornerstone 2025 mental health conference, concluded with remarkable success, solidifying its position as a vital resource for mental health professionals in the region. Founded in 2023 by Jesse Cordova, the conference continues to fulfill its mission of delivering high-quality educational content and essential resources, specifically tailored to address the unique needs of Fort Worth and its surrounding communities.
This year’s 2025 mental health conference delivered a comprehensive 7-hour educational experience, specifically designed for mental health clinicians and practitioners. The event provided a platform for participants to deepen their understanding of critical mental health and substance use issues, while fostering invaluable networking opportunities.
The conference featured a lineup of esteemed speakers, including Lisa Yang, MA, LCDC, CSAT-Candidate; Dr. Brook Keels, PhD, LPC-S; Adry Sanders, LPC-S, CCTP; Sara Shepherd, LCSW; Dr. Chelsea Angelocci, DO; Tanya Stuart, LCSW, BACS, LAC; and Courtney Wilson, LPC.
These experts shared their extensive knowledge and practical insights, covering a range of topics crucial to mental health practices.
Sessions addressed critical areas such as mental health, substance use, networking strategies, the unique challenges faced by Adult Children of Immigrants (ACIs), and adolescent mental health.
The diverse range of topics ensured that attendees gained a well-rounded understanding of current issues and best practices.
The conference facilitated meaningful connections among professionals, fostering a collaborative environment for sharing ideas and resources.
Attendees had the opportunity to engage with representatives from leading clinics and organizations, expanding their professional networks.
The 3rd Annual Resiliency & Recovery Conference of Fort Worth was made possible through the generous support of our sponsors, who are committed to advancing mental health services in the Fort Worth area:
Mind Above Matter

“We are incredibly proud of the impact this year’s 2025 mental health conference has had on our community,” said Jesse Cordova, founder of the Resiliency & Recovery Conference. “The dedication of our speakers, sponsors, and attendees is a testament to the importance of addressing mental health and substance use challenges. We are already looking forward to the 4th annual conference, where we will continue to build on this momentum.”
Attendees are encouraged to stay tuned for updates on the 4th annual conference and to explore the Mind Above Matter website for additional mental health resources.

Grapevine, TX – March 14, 2025 Mind Above Matter Partners with Maples Treatment Center and Meridell Achievement Center to Host Affirmation Box Workshop at House Shine
In celebration of St. Patrick’s Day 2025, participants from Maples Treatment Center and Meridell Achievement Center joined Mind Above Matter in a creative and therapeutic workshop. The focus of the event was to design and create personalized affirmation boxes. These boxes serve as a repository for positive affirmations, encouraging individuals to start their day with a positive mindset.
Participants had the option to write their own powerful daily affirmations or select from a shared pool, adding an element of surprise and community support. The event incorporated the symbolic shamrock, representing luck and positivity, to further enhance the uplifting experience.


The Maples Treatment Center focuses on helping teenage girls struggling with their mental health, including trauma, disordered eating, and/or substance use. They provide a safe place for residents and their families to work together on their unhealthy past decisions. The Maples uses respect, accountability, and self-love to encourage healthier choices.
Their residential program is staffed with trained mental health professionals that provide evidence-based therapies. They offer activities that support structure and accountability while having an environment that promotes creativity, mindfulness, goal setting, and self-care.

The Meridell Achievement Center in Liberty Hill, Texas, is a residential treatment center specializing in behavioral and neurobehavioral programs for adolescents aged 10-17. The center has provided specialized care for children and adolescents for over 60 years.
Meridell treats adolescents with a variety of diagnoses including bipolar disorder, ADHD, PTSD and high-end autism spectrum disorders, among others. Meridell Achievement Center is accredited by the Joint Commission and licensed by the state of Texas. The center also supports the whole family.
Mind Above Matter was honored to collaborate with Maples Treatment Center and Meridell Achievement Center, both renowned for their commitment to mental wellness. These partnerships underscore our shared dedication to providing valuable mental health resources and support to our communities.
The practice of using daily affirmations has been shown to have numerous benefits of affirmations and benefits of positive affirmations. Scientific research supports the notion that regularly affirming positive statements can rewire the brain, reducing stress and increasing feelings of self-worth. Studies indicate that affirmations can activate areas of the brain associated with self-related processing and reward, leading to improved mental and emotional well-being. The scientific benefits of affirmations include:
By creating affirmation boxes, participants are equipped with a practical tool to integrate these benefits into their daily lives.
“We are thrilled to have partnered with Maples Treatment Center and Meridell Achievement Center for this meaningful event,“ said Jesse Cordova, Director of Business Operations at Mind Above Matter. “Creating affirmation boxes is a wonderful way to instill positivity and encourage self-reflection. We are committed to providing resources that support mental wellness and look forward to continuing our work in the community.”
At Mind Above Matter, we believe that everyone deserves access to quality mental health care. If you or a loved one are seeking mental health services, we encourage you to reach out to our team of qualified mental health professionals. We offer a range of services tailored to meet individual needs. To learn more about our offerings and access valuable mental health resources, visit our website today. Our team is here to support you on your journey to mental wellness.
For daily affirmations and mental health tips, follow Mind Above Matter on Instagram, Facebook, and LinkedIn.
We proudly serve Keller and Burleson, Texas as well as multiple Texas school districts including Carrollton Farmers Branch, Irving, and Waxahachie ISDs.
Related Posts: 2025 Resiliency & Recovery Conference of Fort Worth
Spring has sprung, and with it comes a sense of renewal and possibility. Spring’s arrival brings a chance for renewal, and that extends to your mental well-being. This season offers unique opportunities to engage in refreshing mental health activities.
Let’s explore how you can leverage the energy of spring to engage in rejuvenating mental health activities.
Spring’s arrival often brings a natural lift in mood. The increased sunlight triggers the production of vitamin D, a crucial nutrient for mental health. However, this season can also present challenges. Some individuals experience “reverse SAD,” feeling overwhelmed by the surge of social activities and expectations. It’s essential to proactively manage your mental health during this transitional period.
Increased sunlight exposure leads to higher vitamin D production in the body. Vitamin D plays a crucial role in regulating mood by influencing serotonin levels, a neurotransmitter associated with happiness and well-being.
Spending time in nature has been shown to reduce levels of cortisol, the stress hormone. Studies have demonstrated that exposure to natural environments can promote relaxation, improve mood, and enhance cognitive function.

Embrace the outdoors and let nature be your therapist. Engaging in outdoor mental health activities can significantly enhance your well-being.
Grounding and Connection
Immerse yourself in nature by taking a walk or hike. Feel the earth beneath your feet and reconnect with the natural world.
Mindful Walking Tips
Practice mindful walking by focusing on your senses and breathing deeply. Notice the textures of the path, the sounds of birdsong, and the scents of blooming flowers.
Therapeutic Nurturing
Engage in the therapeutic act of gardening or planting. Nurturing plants can be a rewarding experience that fosters a sense of accomplishment and reduces stress.
Creating a Small Garden
Even a small space can become a sanctuary. Create a small indoor or outdoor garden to bring the beauty of nature into your home.
Mood-Boosting Movement
Physical activity is a powerful mood booster. Engaging in outdoor exercise can release endorphins, natural chemicals that have mood-elevating effects.
Spring Activities
Enjoy activities like cycling, jogging, or outdoor yoga. Take advantage of the warmer weather and spend time in nature while getting some exercise.
Setting Realistic Goals
Start small and gradually increase your activity level. Set realistic fitness goals and celebrate your progress along the way.
Sensory Awareness
Practice mindful observation by simply sitting outside and observing nature. Pay attention to the sights, sounds, and smells around you.
Focused Attention
Engage in focused attention by observing a single object or phenomenon in nature, such as a bird, a flower, or a cloud.

Even when indoors, you can cultivate a sense of calm and well-being.
Decluttering and Organizing
Engage in a spring cleaning of your physical and mental space. Decluttering and organizing your living environment can create a sense of calm and reduce stress.
Reducing Stress
A tidy and organized space can promote mental clarity and reduce feelings of overwhelm.
Art Therapy
Engage in creative activities like painting, drawing, or sculpting. Art therapy can be a powerful tool for processing emotions and promoting self-expression.
Writing and Music
Explore writing, journaling, or playing music. These activities can provide a healthy outlet for emotions and promote relaxation.
Processing Emotions
Creative outlets can help you process emotions, gain insights into your thoughts and feelings, and develop a deeper understanding of yourself.
Guided Meditation
Use apps or online resources to guide you through meditation exercises.
Simple Breathing Exercises
Practice simple breathing exercises, such as deep breathing or diaphragmatic breathing, to calm your mind and reduce stress.
Reducing Anxiety
Regular mindfulness and meditation practices can help reduce anxiety, improve focus, and promote overall well-being.
Scheduling Social Time
Make a conscious effort to schedule time for social interaction with friends and family.
Interactive Activities
Plan interactive activities, such as game nights, potlucks, or outdoor picnics, to foster social connection and enjoyment.
Combating Isolation
Social connection is vital for mental health. Make an effort to combat social isolation by engaging in activities that bring you together with others.
Reflect on Growth and Change
Use journaling prompts to reflect on personal growth and change. Consider questions like: “What new things are you looking forward to this spring?” or “How can you grow and change this season?”
Embrace the Feeling of Renewal
Explore the feeling of renewal associated with spring. Write about what renewal means to you and how you can cultivate a sense of renewal in your own life.
Spring offers a unique opportunity to prioritize your mental health. By engaging in these mental health activities, you can cultivate a sense of well-being and resilience. At Mind Above Matter, we’re committed to supporting your mental health journey. Whether you’re seeking individual therapy, family counseling, or educational resources, we’re here to help. Contact our offices or visit our website to learn more about our mental health services and how we can support you this spring and beyond.
We proudly serve Keller and Burleson, Texas and multiple independent school districts including Frisco, Irving, and Waxahachie, Texas.
Related: Summer Mental Health Tips for the Warmer Months
Music is a universal language that transcends cultural boundaries and speaks directly to the soul. From ancient rituals to modern playlists, it has been an integral part of the human experience. But its power extends far beyond entertainment. Music possesses a remarkable ability to influence our emotions, thoughts, and physical well-being, making it a valuable therapeutic tool in mental health.
This article explores the connection between music therapy and mental health, exploring its definition, history, neurological effects, and diverse benefits for individuals seeking mental wellness.
Music therapy is a recognized healthcare profession that utilizes music interventions to address individualized goals within a therapeutic relationship. It’s more than just playing music; it’s a structured, evidence-based practice delivered by credentialed professionals. Music therapists are highly trained to assess each individual’s unique needs and design interventions that may encompass a variety of musical experiences. These can include creating music through songwriting or improvisation, singing familiar tunes, moving to music, actively listening to specific pieces, and engaging in discussions about the emotional responses evoked by music.
The cornerstone of effective music therapy is the therapeutic relationship between the client and the therapist. This relationship provides a safe, supportive, and non-judgmental space for individuals to explore their inner world, express their emotions, develop coping mechanisms, and ultimately improve their overall well-being. Music therapists possess a deep understanding of the psychological, emotional, cognitive, and social impact of music. They leverage this knowledge to guide clients through musical experiences that promote healing and growth.
The use of music for healing dates back to ancient civilizations, but music therapy as a formal profession emerged in the 20th century. Its development was significantly influenced by the profound experiences of musicians who volunteered in hospitals during World Wars I and II. These musicians witnessed firsthand the positive effects of music on patients’ emotional and physical states, observing how it could alleviate pain, reduce anxiety, and foster a sense of connection during times of great hardship.
Fueled by these observations, formal training programs in music therapy began to take shape, and the profession gradually gained recognition within the broader healthcare field. Over the ensuing decades, rigorous research has continued to expand our understanding of the therapeutic benefits of music. This growing body of evidence has led to the increasing integration of music therapy into a wide array of treatment settings, including mental health facilities, general hospitals, rehabilitation centers, schools, community centers, and private practices.
The human brain exhibits a complex and fascinating response to music. Advanced neuroimaging studies have revealed that listening to or creating music activates a multitude of brain regions simultaneously. These regions are intricately involved in processing emotions, cognition, sensory information, and motor control. This widespread and integrated brain activity is believed to play a crucial role in the therapeutic effects of music.
Music has the power to influence the release of various neurotransmitters, which are chemical messengers in the brain. For example, it can stimulate the release of dopamine, a neurotransmitter associated with pleasure, motivation, and reward. This can explain why music can be effective in elevating mood and fostering a sense of well-being. Conversely, music can also help regulate the release of cortisol, a hormone associated with stress. This can contribute to its ability to reduce anxiety and promote relaxation. Furthermore, music has been shown to enhance neural plasticity, the brain’s remarkable ability to reorganize itself by forming new neural connections. This is a critical process for learning, memory, and recovery from neurological conditions.
Music therapy offers a diverse range of benefits for individuals seeking to improve their mental health. One of its most powerful attributes is its capacity to provide a non-verbal outlet for emotional expression. This can be particularly valuable for individuals who struggle to articulate their feelings verbally, such as those who have experienced trauma, have communication difficulties, or are navigating complex emotions. Music can offer a safe and creative way to communicate and process these emotions.
Beyond emotional expression, music is a potent tool for stress reduction. Listening to calming music can elicit physiological changes, such as slowing down the heart rate, lowering blood pressure, and reducing muscle tension. Music therapy interventions can equip individuals with relaxation techniques and coping skills that they can use to manage stress and anxiety in their daily lives. In addition, music therapy can enhance self-esteem and confidence, improve social skills and interaction, and foster a sense of connection and belonging, particularly in group therapy settings.

Depression can significantly impair mood, motivation, and overall quality of life. Music therapy provides a supportive and engaging avenue for individuals to explore and process the complex emotions associated with depression, such as sadness, hopelessness, and anger. Interventions may include songwriting, lyric analysis, listening to emotionally resonant music, and playing instruments. These activities can help individuals express their feelings in a healthy way, increase motivation, promote social interaction, and cultivate a sense of hope and empowerment.
Attention-deficit/hyperactivity disorder (ADHD) is characterized by challenges with attention, impulsivity, and hyperactivity. Music therapy can offer structured and engaging strategies to improve focus, self-regulation, and cognitive function in individuals with ADHD. Interventions may incorporate structured drumming activities to enhance attention span, movement and music to release excess energy and improve coordination, and songwriting to express emotions and develop communication skills. The rhythmic and predictable nature of music can provide a sense of organization and structure, which can be particularly beneficial.
Autism spectrum disorder (ASD) can affect communication, social interaction, and sensory processing. Music therapy offers a unique and effective way for individuals with ASD to enhance communication, social skills, and emotional expression. Interventions may involve singing, playing instruments, improvising music, and using music to facilitate social interaction and connection. Music can provide a predictable and engaging medium for communication, allowing individuals with ASD to connect with others and express themselves in novel and meaningful ways. Music therapy can also aid in sensory integration and reduce anxiety.
The versatility of music therapy extends to a wide range of other mental and physical health conditions. For individuals with Parkinson’s disease, music therapy can be used to improve motor skills, gait, and speech. The rhythmic cues inherent in music can help regulate movement and enhance coordination. In Alzheimer’s care, music therapy can be a powerful tool to evoke memories, reduce agitation, and improve mood in individuals with dementia. Familiar songs can tap into preserved cognitive functions and provide a sense of comfort and connection. Music therapy is also utilized in pain management, rehabilitation programs, and end-of-life care.

Music therapy encompasses a variety of approaches and techniques, each tailored to the specific needs of the individual or group.
At Mind Above Matter, we recognize the profound therapeutic value of creative expression. In addition to our other mental health services, we offer weekly music and art therapy programs at our clinics in Keller and Burleson, Texas. These programs provide a unique and engaging way for individuals to explore their feelings, develop coping skills, and enhance their overall quality of life. Our music therapy offerings include group therapy sessions, providing a supportive and collaborative environment for individuals to connect with others and express themselves through music. We also provide specialized children’s music therapy programs, tailored to the developmental needs and challenges of adolescents as young as 9. All of our music and art therapy programs are facilitated by licensed professionals holding a music therapy license, ensuring a high standard of care and clinical expertise.
Music therapy offers a powerful and effective approach to promoting mental wellness. From its capacity to facilitate emotional expression to its positive impact on brain function, music has a significant role to play in supporting individuals on their journey to healing and growth. For more detailed information on music therapy, please visit the American Music Therapy Association website.
If you or someone you know could benefit from music therapy or other mental health services, we encourage you to reach out. Our team at Mind Above Matter is here to provide compassionate and effective care. Contact us today to learn more about our programs and how we can support your journey to well-being.
Related Links: Creating Connections: The Benefits of Group Therapy
The impact of trauma is a deeply personal and multifaceted experience. Recognizing the diverse ways in which individuals are affected, the mental health field has established a comprehensive framework known as the five levels of trauma care.
This tiered system ensures that individuals receive support tailored to the intensity of their experiences and their unique needs, guiding them on a path toward healing and recovery. Understanding these levels can provide clarity for those seeking help and empower professionals to deliver the most effective and compassionate care.
A tiered approach to trauma care acknowledges that not all traumatic experiences have the same impact, and individuals will require varying levels of support. This system prevents a one-size-fits-all approach, which can be ineffective or even re-traumatizing.
By matching the intensity of the intervention with the individual’s level of distress and the complexity of their trauma history, this framework optimizes the healing process. It emphasizes a continuum of care, allowing individuals to access the right support at the right time, progressing through levels as needed.
The initial level of trauma care focuses on providing individuals with fundamental knowledge about trauma and its common effects. This stage empowers individuals to understand their reactions and utilize self-help strategies to manage their well-being. Often suitable for those who have experienced potentially traumatic events but aren’t currently facing significant distress or impairment, Level 1 aims to build resilience and normalize the recovery process.
Psychoeducation at this level involves offering accessible information about the body’s stress response, typical trauma symptoms like sleep disturbances and anxiety, and the general trajectory of healing. Resources such as informative websites, self-help books, and introductory workshops can provide a broad understanding of trauma’s impact.
Self-help strategies are a cornerstone of Level 1 care. These often include teaching basic stress management techniques such as relaxation exercises and mindfulness practices. Developing healthy lifestyle habits – regular exercise, balanced nutrition, and sufficient sleep – are also emphasized as they significantly contribute to overall mental and emotional resilience.
Moving beyond foundational knowledge, Level 2 trauma care offers more direct support through brief interventions and early support systems. This level is designed for individuals experiencing mild to moderate distress or functional challenges in the aftermath of a traumatic event. Brief therapy models, crisis counseling, and peer support groups facilitated by trained professionals are common interventions.
Brief therapy approaches at this stage are typically time-limited and focus on addressing specific symptoms or developing immediate coping skills. Crisis counseling offers immediate support during or shortly after a traumatic event, helping individuals regain a sense of safety and emotional equilibrium.
Support groups provide a vital space for individuals with shared experiences to connect, offer mutual understanding, and learn from one another. This sense of community can be incredibly validating and help normalize trauma responses in the early stages of recovery.
Level 3 trauma care involves more intensive and sustained outpatient therapy for individuals who have developed trauma-related disorders, such as PTSD, Acute Stress Disorder, or those grappling with the effects of childhood trauma therapy. This level utilizes evidence-based psychotherapies specifically tailored to address the complex psychological and emotional sequelae of trauma. The primary goals include processing traumatic memories, reducing intrusive symptoms, addressing avoidance behaviors, and enhancing emotional regulation skills.
Common therapeutic modalities employed at this level include cognitive behavioral trauma therapy (CBT-T), Eye Movement Desensitization and Reprocessing (EMDR), and other trauma-informed approaches. These therapies guide individuals through the careful and gradual processing of traumatic experiences within a safe and supportive therapeutic relationship.
Therapists at this level are skilled in helping individuals manage intense emotions, develop effective coping mechanisms for trauma triggers, and challenge negative, trauma-related thought patterns. The overarching aim is to facilitate deep healing, reduce the severity of symptoms, and improve overall daily functioning and quality of life for those impacted by trauma.
Level 4 trauma care offers more intensive and structured treatment through Intensive Outpatient Programs (IOPs) and Partial Hospitalization Programs (PHPs). These programs provide several hours of therapy multiple days a week, offering a significantly higher level of support and structure compared to traditional weekly outpatient therapy. This level is often beneficial for individuals experiencing substantial functional impairment, high levels of distress, or those requiring more intensive stabilization and skill-building. This can be particularly helpful for individuals requiring attachment trauma treatment or navigating the complexities of complex trauma treatment.
IOPs and PHPs for trauma integrate various therapeutic modalities, including individual therapy, group therapy, psychoeducation, and skills training focused on emotional regulation and coping strategies. Multidisciplinary teams, comprising therapists, psychiatrists (for medication management when necessary), and other mental health professionals, collaborate to create and implement personalized treatment plans. This intensive level of care provides a supportive and structured environment crucial for addressing significant trauma-related challenges and fostering stabilization.
The most intensive level of trauma care, Level 5, involves treatment within inpatient or residential settings. This level is reserved for individuals experiencing severe trauma-related symptoms that pose a significant risk to their safety or severely impair their ability to function in daily life. This may include those in acute crisis, at high risk of self-harm or harming others, experiencing severe dissociation, or managing complex co-occurring mental health and substance use disorders. The primary focus is on providing a secure and contained environment for immediate stabilization, intensive therapeutic intervention, and comprehensive crisis management.
Inpatient and residential trauma programs offer continuous 24/7 support and supervision, alongside intensive individual and group therapy, psychiatric care, and medical management. The goal is to stabilize acute symptoms, ensure the safety of the individual, and initiate the process of addressing the underlying trauma within a highly structured and supportive setting. The duration of stay in these programs is tailored to the individual’s unique needs and progress. Following this intensive phase, individuals typically transition to a lower level of care to continue their journey of recovery.
Navigating the complexities of trauma requires a nuanced and individualized approach. Understanding the five levels of trauma care provides a roadmap for both individuals seeking support and professionals dedicated to facilitating healing. Recognizing the different levels ensures that individuals receive the appropriate intensity of care, fostering resilience and promoting lasting recovery.
If you or someone you know is seeking support on their journey to healing from trauma, Mind Above Matter offers a range of outpatient therapy services at our locations in Keller and Burleson, Texas. We also provide virtual therapy services throughout Texas. We are committed to providing accessible and compassionate care to support your mental well-being.
Related: What are the 5 Levels of Trauma Care?
MIND ABOVE MATTER SPONSORS DENTON NEIGHBORS NETWORK EVENT
Denton, TX – May 28, 2025 – Mind Above Matter, a leading provider of comprehensive mental health services in Texas, proudly sponsored the Denton Neighbors Network monthly mental health networking event yesterday, May 28, 2025. Held at Patchouli Joe’s Bookstore, the gathering brought together a diverse group of mental health professionals dedicated to strengthening community-based care.
The event, hosted monthly by Neighbors Counseling in Denton, serves as a vital platform for creating a robust network of mental health providers. Its core purpose is to facilitate client referrals, encourage discussions on best practices and new treatment methods, and foster the sharing of essential resources. As this month’s sponsor, Mind Above Matter was given the opportunity to highlight its extensive services, including its outpatient programs in Keller and Burleson, and its innovative iMatter school-based mental health program.

Attendees included a wide array of professionals, such as therapists, business development representatives, school advocates, and representatives from organizations like NAMI. The collaborative atmosphere underscored the collective commitment within the mental health community to enhance access to care and ensure individuals receive the most appropriate treatment. By fostering these relationships, Mind Above Matter continues its mission to close the gap in mental health care and treatment across Texas.

“We were thrilled to sponsor the Denton Neighbors Network event and engage with so many passionate professionals committed to mental wellness,” said Tracie Owen, Community Relationships Representative. “These collaborative efforts are essential for building stronger referral pathways and ensuring that individuals and families in our communities receive the comprehensive support they need, whether through our clinic-based services or our school programs.”
About Mind Above Matter: Mind Above Matter is a dedicated mental health organization providing comprehensive outpatient therapy services for adolescents and adults across Texas, with brick-and-mortar locations in Keller and Burleson. Offering Partial Hospitalization Programs (PHP), Intensive Outpatient Programs (IOP), individual therapy, medication management, and specialized programs like the iMatter school-based mental health initiative, Mind Above Matter is committed to delivering accessible, high-quality, and compassionate care to promote lasting well-being.
Related: 2025 St. Patty’s Day Affirmation Box Workshop
The last bell rings, textbooks are shelved, and the doors swing open to a season of sunshine and freedom. For many students, summer break is synonymous with fun and relaxation. However, beyond the obvious joys of vacations and late mornings, this extended pause in the academic year plays a profoundly critical role in fostering positive mental health. In an era where academic pressures are escalating, understanding why summer break is good for students’ mental health is more important than ever.
Today’s students navigate a high-pressure environment, juggling demanding curricula, the intensity of standardized testing, a packed schedule of extracurricular activities, and complex social dynamics. This constant state of high-alert performance can lead to significant stress, anxiety, and even burnout, impacting not just academic performance but overall mental well-being. The relentless pace leaves little room for minds to genuinely unwind and recharge.
Summer break, therefore, emerges as a vital period for mental health rejuvenation. It’s a necessary pause in the academic cycle that allows students to disconnect from stressors, reconnect with themselves, and engage in activities that foster well-being. Today, we will explore the key benefits of summer break, highlighting how these contribute to a healthier, more balanced mental state for students.
The structured and often demanding environment of school can lead to chronic stress in students. From the cognitive load of constantly learning new material to the pressure of deadlines and the intricate social dynamics of school life, a student’s brain is under constant mental exertion. Summer break offers a crucial respite, allowing the mind to decompress from this continuous intellectual and emotional demands. This period of reduced demands helps to lower cortisol levels, the body’s primary stress hormone, and effectively resets the body’s stress response system.
This reduction in stress directly contributes to preventing burnout, a state that can manifest in students as emotional exhaustion, a cynical attitude towards school, and a diminished sense of personal accomplishment. When students are burnt out, their motivation wanes, and their capacity to engage with learning or social activities decreases significantly. Summer provides the essential time needed for students to genuinely recharge their mental batteries, regaining their natural curiosity, enthusiasm, and motivation for the upcoming academic year. It’s not just a break; it’s a profound opportunity for their minds to rest and recover.
In modern childhood and adolescence, the role of unstructured play has unfortunately diminished, often supplanted by highly organized activities, scheduled lessons, and extensive screen time. Summer break naturally opens up invaluable opportunities for free play, where students can explore their interests without external rules, performance expectations, or the pressure to achieve a specific outcome. This type of play, characterized by self-direction and intrinsic motivation, is vital for developing crucial skills such as problem-solving, emotional regulation, and social competencies outside of a structured environment.
Moreover, this period of unstructured time actively nurtures creativity. When students are not bound by rigid curriculum guidelines or specific assignments, their minds are free to wander, experiment, and imagine. This freedom allows them to delve deeper into personal hobbies, read for pure pleasure, or simply engage in imaginative thinking without constraints. Such activities are crucial for fostering cognitive development, emotional expression, and a healthy sense of self. Summer truly provides a fertile ground for self-discovery and innovation that is often curtailed during the school year.
The demanding schedules of school often lead to widespread chronic sleep deprivation among students. Early start times, coupled with hours dedicated to homework, participation in numerous extracurricular activities, and the pervasive presence of social media, frequently result in insufficient and irregular sleep patterns. This chronic lack of quality sleep significantly impairs a student’s cognitive function, hinders their ability to regulate emotions, and diminishes their overall mental resilience, making them more susceptible to stress and anxiety.
Summer break provides the ideal opportunity to reset these disrupted sleep patterns. With fewer fixed obligations like early alarms or late-night study sessions, students can naturally adjust to a more aligned circadian rhythm, allowing them to achieve the adequate and restorative rest that their developing brains and bodies desperately need. Improved sleep directly translates to a more positive mood, reduced irritability, enhanced concentration, and a stronger, more effective ability to cope with stressors when they return to school. This natural recalibration of sleep cycles is a cornerstone of mental well-being.
While school life inherently offers continuous social interaction, it can also paradoxically be a significant source of social pressure, constant peer comparison, and even bullying, which can negatively impact a student’s self-esteem and mental health. Summer break provides a welcome opportunity for students to broaden their social horizons beyond the immediate school environment. They can connect with friends from different social circles, forge new bonds in less competitive settings, or simply spend more quality, relaxed time with family members without the underlying tension of academic schedules. This diversification of social interactions can significantly reduce social anxiety and pressure often associated with school dynamics.
Furthermore, the increased free time during summer facilitates deeper engagement with family members through shared activities, travel, or simply more spontaneous interactions. It also opens doors for participation in community events, volunteering, or enrolling in summer camps, fostering new friendships and a stronger sense of belonging outside of academic settings. These varied and often lower-pressure social interactions are crucial for healthy social-emotional development, teaching students different forms of communication and connection that contribute to their overall mental well-being.
The typical school day often necessitates prolonged periods of sitting in classrooms, leading to a largely sedentary lifestyle for many students. This pervasive lack of consistent physical activity can profoundly impact mental health, contributing to feelings of sluggishness, a diminished mood, and decreased energy levels, which can exacerbate existing emotional challenges.
Summer break naturally encourages more outdoor time and increased physical activity. Whether it’s through organized sports, swimming, hiking, cycling, or simply spending leisurely time in nature, increased movement and exposure to natural environments are proven mood boosters. Direct sunlight exposure contributes to the body’s production of Vitamin D, which plays a role in mood regulation, and helps regulate serotonin levels in the brain. Moreover, physical activity is a powerful stress reliever and a natural antidepressant. Connecting with nature fosters a profound sense of calm, reduces rumination, and enhances overall well-being, further solidifying the link between physical and mental health.
In conclusion, summer break serves as far more than just a simple vacation from school. It is a critical period that offers a holistic rejuvenation for students’ mental health. By providing essential opportunities for stress reduction, fostering unstructured play and creativity, improving sleep patterns, enhancing social connections beyond school, and promoting crucial physical activity and engagement with nature, summer break plays an indispensable role in a student’s overall well-being. This period of essential reset and growth allows young minds to decompress, rebuild resilience, and develop crucial coping mechanisms.
Ultimately, students who fully embrace these myriad benefits are far more likely to return to school feeling refreshed, resilient, and better equipped to handle the academic and social challenges of the coming year. At Mind Above Matter, we understand the profound impact of mental health on every aspect of a student’s life. We are proud to offer comprehensive mental health services in Keller and Burleson, Texas. We also deeply value our partnerships with Frisco ISD, Irving ISD, and Waxahachie ISD to provide essential student mental health services even during summer break, ensuring continuous support. If you or a student in your life needs mental health support, please visit our dedicated iMatter service page for more information.
Related Links: Refreshing Spring Mental Health Activities
DENTON, TX — Mind Above Matter (MAM), a leading provider of restorative behavioral health services in North Texas, is proud to announce a new partnership with Denton Independent School District. This collaboration introduces the IMatter program to the district, with a primary clinical site established at Fred Moore High School.
The IMatter program is an integrated, school-based initiative designed to meet students exactly where they are. By providing Partial Hospitalization (PHP) and Intensive Outpatient (IOP) levels of care directly within the district community. IMatter bridges the critical gap between traditional weekly therapy and inpatient hospitalization.
“Our mission is to help students navigate their emotional challenges in a familiar, reassuring environment,” said Joann Gillen, Executive Director of IMatter. “By integrating our clinical team into the Denton ISD community, we ensure that students don’t have to choose between their education and their mental health. We are bringing them one step closer to whole.”
The IMatter program at Fred Moore High School offers:
This partnership addresses a growing need for accessible adolescent mental health services in North Texas. IMatter provides students with concrete coping strategies and behavioral support to stabilize in crisis and foster long-term resilience within the classroom.
For more information about the IMatter program, please visit www.mindabovematter.com or contact [email protected].
About Mind Above Matter
Mind Above Matter provides restorative, full-circle mental health care across North Texas. Through their specialized IMatter school partnerships and clinical facilities, they are dedicated to helping adolescents and adults move closer to whole. With a focus on clinical integrity and compassionate support, Mind Above Matter is redefining the path to mental wellness.